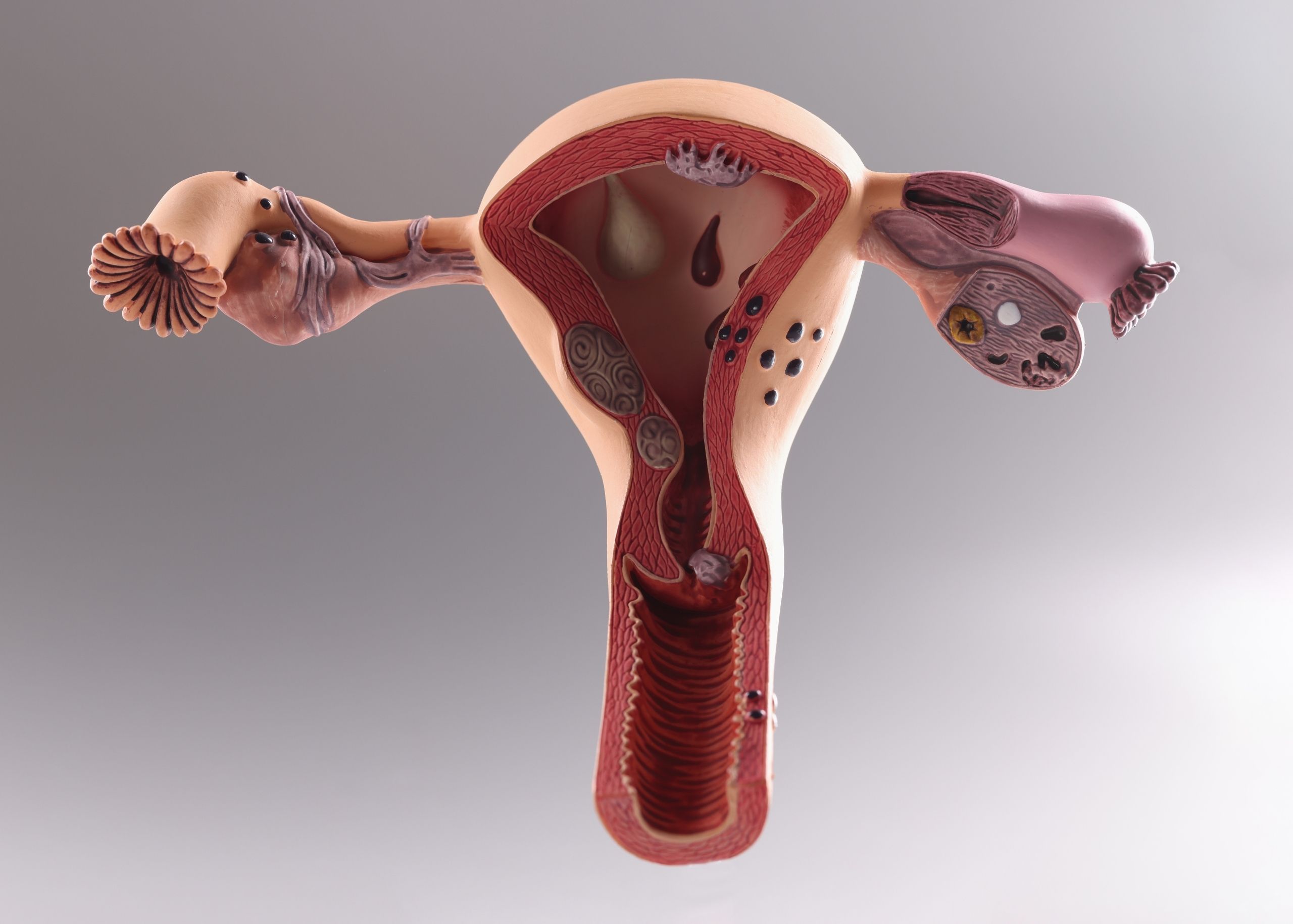
Kidney stones are hard deposits that form within the kidneys. They can cause a lot of pain and make it difficult to urinate. They are made from substances like calcium and can be as small as a grain of sand or as big as a golf ball. They often result from a buildup of minerals in the urine. The most common type of kidney stone is made up of calcium, but other substances may also be present.
Most of them pass spontaneously within days or weeks, especially if you drink plenty of liquids and increase your water intake. However, if you have recurrent kidney stones, surgery might be necessary to remove them permanently or prevent their recurrence. It is essential to let your Urologist know if you’ve had any symptoms here.
Types of Kidney Stones
Kidney stones can be divided into four main types: calcium oxalate, calcium phosphate, uric acid, and struvite.
- Calcium oxalate stones are the most common type. They form when calcium combines with oxalate in urine
- Calcium phosphate stones form when calcium combines with phosphorus to form crystals that then become hard material in your kidneys. Doctors don’t know why this happens
- Uric acid stones are caused by excess uric acid in your system. The acid makes its way into your urine and forms crystals there. These crystals bond together to create a stone that can block your urinary tract
- Struvite stones. A bacterial infection caused in your urinary tract or bladder
- Cystine: They are Rare. They occur in both men & women who have the genetic disorder cystinuria
Causes of Kidney Stones
They occur when there is an imbalance in the number of minerals in the urine. The minerals crystallize and form crystals that stick together to form a stone. The crystals can become stuck in the kidney, ureter (the tube that connects the kidneys to the bladder), or bladder. This causes pain and other symptoms, such as nausea and vomiting, blood in urine, frequently urinating and feeling like you need to go. Still, nothing comes out when you do, needing to use the bathroom urgently but having trouble getting there quickly enough.
Warning Signs of Kidney Stones
The following are some of the warning signs:
- Pain in your side or back that is worse when you urinate, or pain while passing urine
- Bloody or cloudy urine
- A feeling that you need to urinate but can’t
- Pain while urinating
- Nausea or vomiting
Risk Factors of Kidney Stones
The risk factors include,
- Gender: Men are twice at risk than women. This may be due to differences in hormones or diet between men and women
- Age: People over the age of 40 are more likely to have the condition
- Family History: Having a family history of the condition increases the chances
- Diet: If you eat a diet high in protein or salt, you may be more likely to develop them
- Conventional treatment for high blood pressure, such as calcium channel blockers, angiotensin II receptor blockers, or thiazide diuretics
Are Kidney Stones Dangerous?
Most of them pass out of your body on their own within several days to two weeks, but they can sometimes be serious if they block one of your urinary tracts or if they cause an infection in your kidneys or bladder. If you have these symptoms, it’s important to see a kidney specialist immediately because they that don’t pass on their own can cause permanent damage to your kidneys.
Foods That Can Cause Kidney Stones
While there are no foods that directly cause them, there are some that may increase your risk and others that may help prevent them from forming.
They often form when the urine contains too much calcium, oxalate, or uric acid. Foods high in these compounds can increase your risk of developing kidney stones by increasing the amount of these compounds in your urine. The following foods are high in calcium, oxalate, or uric acid:
- Calcium-rich foods include milk, cheese, yogurt, and other dairy products. Calcium is also present in bones and other animal-based products such as meat and poultry (including fish). Low-fat dairy products contain less calcium than full-fat versions; however, they still contain enough calcium to increase the risk for stone formation if consumed regularly over time (more than two cups per day)
- Oxalate-rich foods include spinach, beets, and rhubarb; while they won’t cause immediate side effects like pain or discomfort due to their low oxalate content when eaten alone (about 1/2 cup cooked), they can compound problems when combined with other foods high in oxalates like strawberries and chocolate chips
- Animal protein-rich food like meat, fish, egg, and cheese is one of the important causes of uric acid stones if eaten daily and in excess quantity
- Salt (Sodium Chloride) rich foods or salty foods, if eaten in excess the level of sodium raises the amount of calcium in urine which sticks to oxalate in the kidneys that can produce stones
Foods Than Can Help in Preventing Kidney Stones
There are many foods that can help prevent kidney stones, including:
- Tofu contains calcium and magnesium that help prevent the formation of calcium oxalate stones
- Dried figs contain citric acid and have high water content. Citric acid is believed to dissolve the crystals that form in urine, preventing the formation
- Cranberries contain potassium and magnesium, as well as malic acid. Malic acid is believed to prevent calcium from settling in the kidneys and forming crystals which could lead to kidney stones. Cranberries also have high water content and are low in calories and sugar
- Prunes are another fruit with malic acid that can help prevent renal calculi. They also contain iron for anemia prevention, fiber for digestion health, and antioxidants for overall health benefits
- Watermelon is an excellent source of vitamin C which helps prevent calcium oxalate stones from forming in the kidneys or urinary tract system by neutralizing acids in urine which may cause those crystals to form there instead of passing through without being absorbed into our bodies or bloodstreams at all where they could cause health problems including urinary tract infections (UTIs), and gout
Kidney Stone Diagnosis
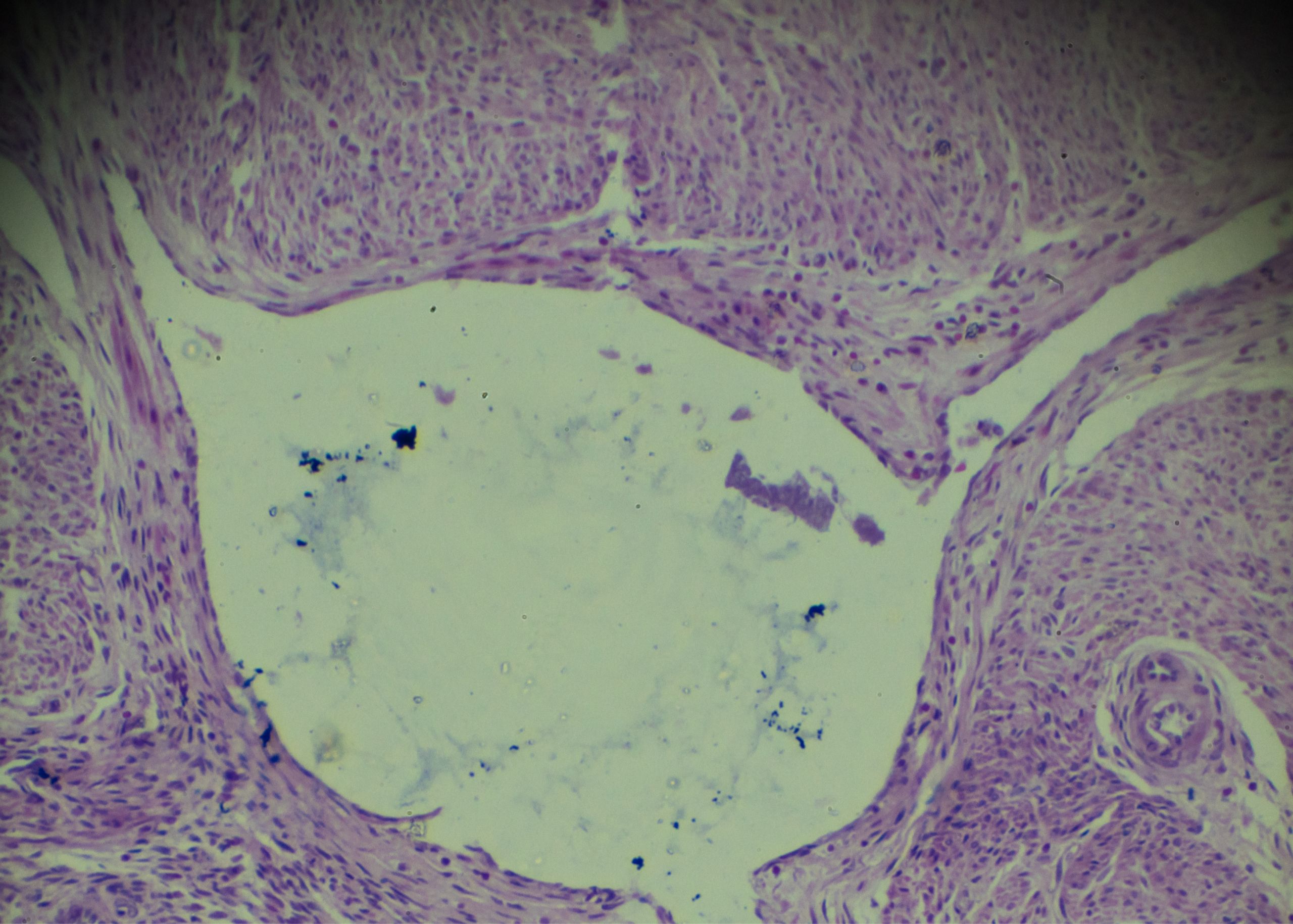
Kidney stones are diagnosed using a physical exam, lab tests, and imaging.
A physical exam includes an abdominal exam, where the doctor presses on your abdomen to feel for a kidney stone. If they can’t feel it, they may order an ultrasound or CT scan to try and pick up the stone.
The lab tests used to diagnose kidney stones include blood tests for electrolyte levels, urinalysis and urine culture because most urinary tract stones accompany by hematuria or urinary infection. The urine culture detects any bacteria that may be causing the infection that leads to kidney stones.
Finally, imaging is used to see if there are any signs of stones in your urinary tract. Your kidney doctor may order an Ultrasound, X-ray, or CT scan to look for any calcifications or other visible signs of possible stones in your kidneys or bladder.
Preventing Kidney Stones
The good news is that there are simple steps you can take to decrease your risk of forming kidney stones:
- Drink plenty of water every day
- Avoid foods that are high in oxalate
- Don’t overdo it on calcium supplements or antacids that contain calcium
- Reduce the amount of salt you eat and drink, if possible
- Get enough exercise each week
- Get enough magnesium and vitamin D in your diet or through supplements; these nutrients help prevent the formation of kidney stones
Learning about your options for treating and preventing kidney stones can make it easier to manage them when they occur. If you think you have kidney stones, see a kidney specialist right away.
Best Treatments for Kidney Stones
Kidney stones are a common medical condition that can be treated with medication, lithotripsy, or surgery.
Medication: The doctor may prescribe medications to help prevent kidney stones from developing or from making them pass more easily.
Lithotripsy: This is a non-invasive treatment for kidney stones. It uses shock waves to break up the stone into smaller pieces that can be passed in the urine. In some cases, the shock waves can leave small fragments of stone in your kidneys or urinary tract. These fragments may need to be removed by surgery.
Surgical Therapy: There are several surgical options available for treating kidney stones in different locations within the urinary system:
Nephrolithotomy Kidney – used to remove small stones from the kidney’s interior
Pyelolithotomy Renal Pelvis – used to remove larger stones from the bottom of the kidney surrounding its ureter (the tube connecting the kidney and bladder)
Ureterolithotomy (ureter) – used to remove large stones stuck in your ureters (tubes connecting each kidney and bladder)
Our Expert Urologist

Dr. Ahmad Mbadda
Specialist Urology
Burjeel Medical Center, Al Shamkha