Causes and Risk Factors of Rotator Cuff Tear
A primary cause of tear of the rotator cuff is the natural wear and tear of tendons with age. This wear occurs from the age of 45. Statistics show that the rupture of the shoulder tendon affects 20% of people over 65 and 50% of people over 80. In addition, several factors can aggravate the natural wear of this cap, namely:
- the current practice of a specific activity requiring a strong solicitation of the shoulder, such as in sports and other repeated activities, as mentioned above
- smoking (resulting in the clogging of the arteries supposed to irrigate the muscles of the shoulder)
- diseases such as diabetes
- anatomy of the shoulder favoring natural wear
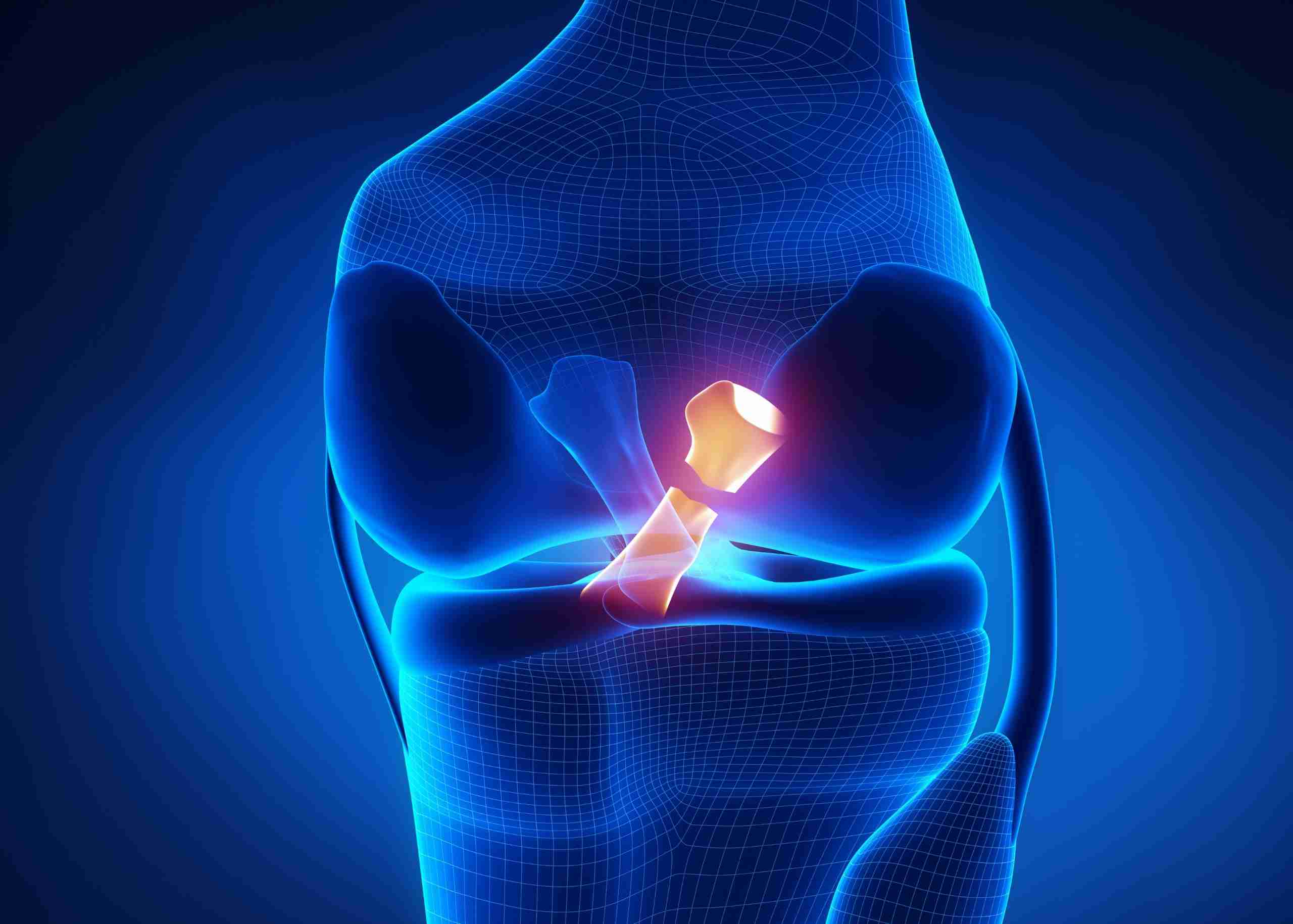
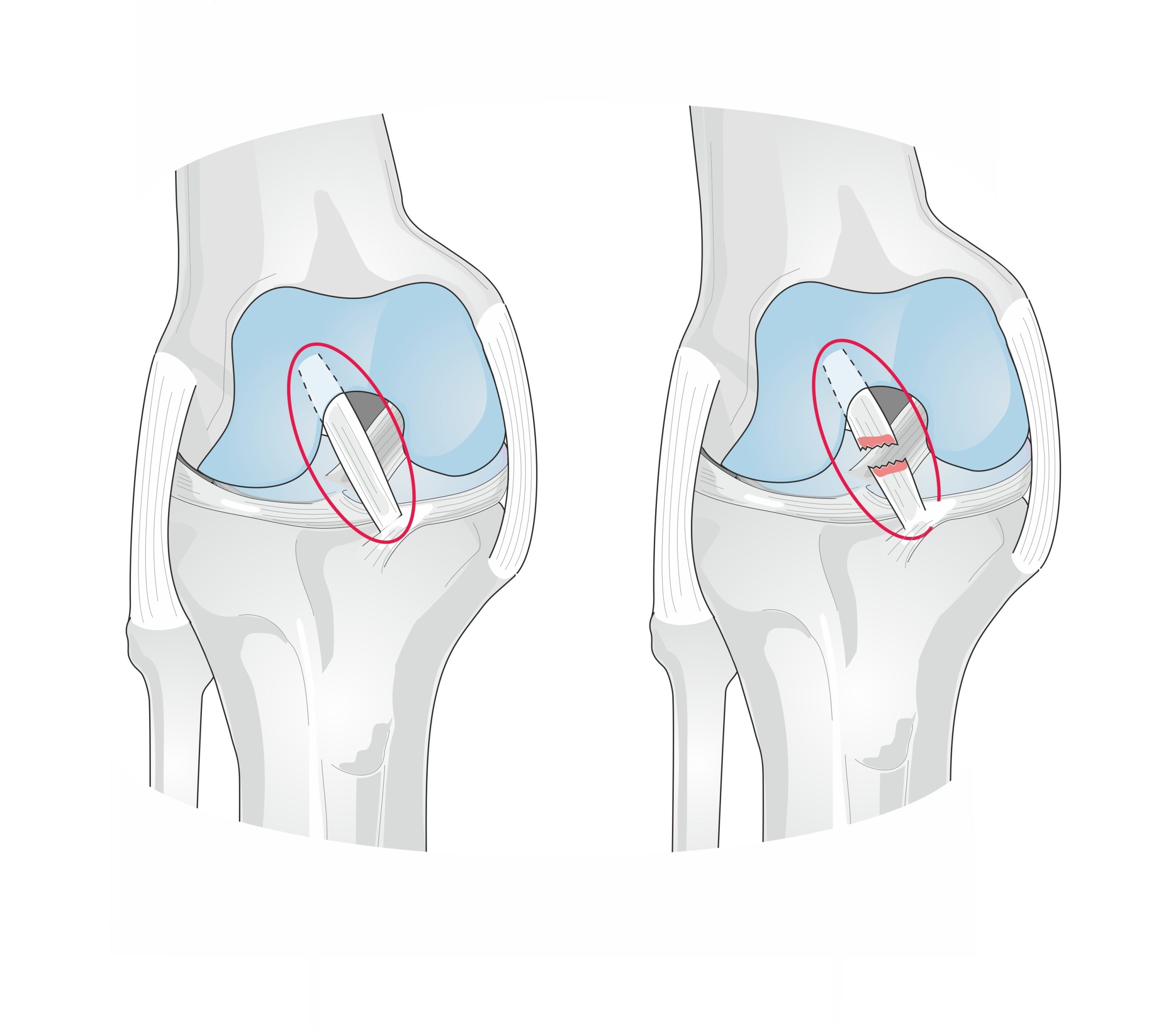
The rupture is the last phase of the subacromial syndrome. It happens when the space between the humerus head and the acromion is narrowing. The rotator cuff tendons (mainly the supraspinatus tendon) are located in this space, protected from the acromion bone by a bag. This bag is known as the subacromial bursa.
The decrease in this space has many causes. The most frequent one is the anatomical constitution of your shoulder (hook-shaped acromion, calcification of the Cossack-acromial ligament, etc.). If we add the repeated movement along the years, it produces a progressive rupture due to the collision between the supraspinatus and the acromion. On the other hand, unlike other tendons in the body, this tendon has very little self-repair capacity in the face of degenerative changes.
In addition to this slow rupture mechanism, there are also traumatic ruptures, in which the tendon ruptures after a fall with an outstretched arm: acute supraspinatus rupture. Sometimes, the rupture of the rotator cuff occurs following a simple and innocuous gesture or a false movement (more common in people over 50). This is called trophic rupture of the shoulder tendon and can also happen to athletes and sports performers.
Rotator Cuff Tear Diagnosis
The diagnosis of complete rupture of the supraspinatus tendon is initially clinical and with imaging tests. The person who presents a rotator cuff tear complains of pain in the shoulder, especially with mobilizations and often pain at night or the inability to lift the arm correctly.
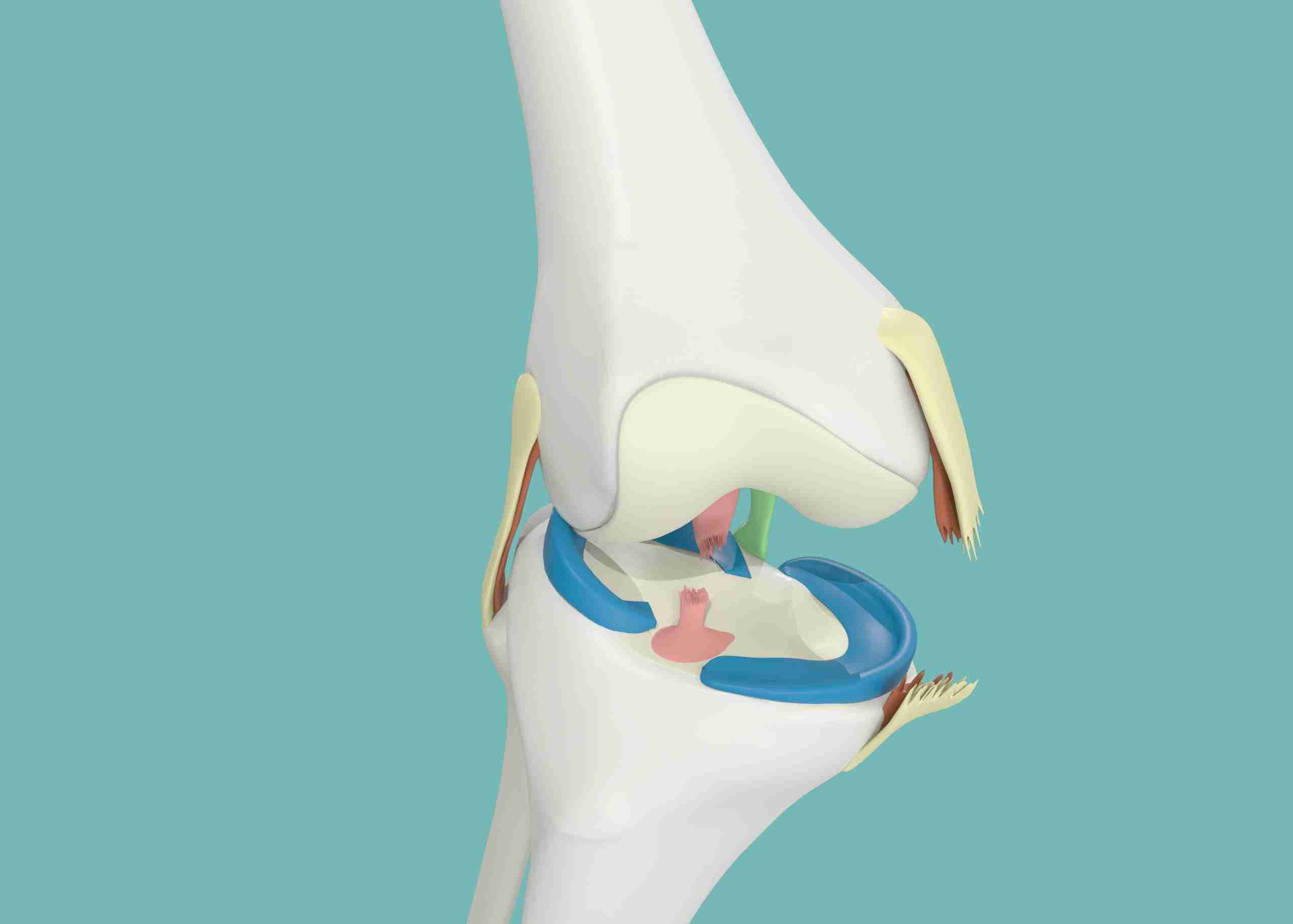
The main diagnosis of tear of the rotator cuff is through a shoulder MRI. The MRI shows us the rupture of the tendon. It also gives us information about the gap or space of the rupture and if there is atrophy or loss of musculature. This also informs about the condition of other tendons, such as the subscapularis or infraspinatus.
Ultrasound is another diagnostic test that, in good hands, allows good visualization of the tendon and the rupture of the supraspinatus. Through it, we can obtain other fundamental data, including:
- Affected tendon(s): Usually supraspinatus or supraspinatus accompanied by infraspinatus or subscapularis
- State of the tissue and the tear: This information is essential to decide the treatment and if the tear is “repairable.”
- Involvement of other structures such as articular cartilage and the long tendon of the biceps
With all this information plus the time of evolution and the symptoms, the doctor will propose a conservative treatment of the rupture (without repairing it) or a surgical repair by arthroscopy to the patient.
Rotator Cuff Tear Treatment
Usually, it is recommended to carry out a sequential treatment in 3 phases.
- Phase 1 treatment with rehabilitation or physiotherapy
- Phase 2 treatment with infiltrations
- Phase 3 treatment with surgery
Non-Surgical Treatment
The aim is to recover the shoulder function (mobility and strength) as much as possible, dispensing with the ruptured tendon. The tendon will be broken, but the Orthopedic doctor will try to increase the rest of the muscles in the area to get closer to the state we had before the muscle broke.
It is recommended to start with a rehabilitation/physiotherapy treatment. There are many exercises and guidelines to recover after a partial tear in the rotator cuff. It is important to note that the exercises must be performed daily for the treatment to have an effect. Usually, it is a 6-12 week program performing cuff strengthening exercises five days a week.
The objective of the initial guideline through exercises or recovery is to achieve the correct shoulder mobility and strengthen the muscles surrounding the shoulder to achieve muscular stabilization of the shoulder. One of the causes of the rupture is the lack of synchronization or correct functioning of the articulation.
Analgesics are used for the initial pain, including corticosteroid injections, to reduce inflammation and pain. If physiotherapy has not effectively improved pain, the doctor can recommend the infiltration of hyaluronic acid.
Surgical Treatment
Shoulder arthroscopy is done in cases where it is decided to perform a rotator cuff tear repair due to the patient’s characteristics (active and in good general condition) and the tear (good tissue, little muscle shortening).
Shoulder arthroscopy is performed, and the tendon rupture is sutured using several anchors that join the tendon to the bone.
In this intervention, several surgical procedures are performed at the same time, all through 2 or 3 small incisions (less than 1cm)
- Remove the inflamed bursa: Bursectomy
- File the thickened acromion to increase the space in cases where it is: Acromioplasty
- Repair the break: Cuff Suture
This repair is done by placing implants in the humerus (made of titanium or other biocompatible materials) to which strong tension-resistant sutures are attached. In cases of partial ruptures, it is often necessary to complete the tear and move the entire released tendon back to its original insertion site, which the surgeons join with one of the harpoons (implant).
In the case of total ruptures of one or two tendons, several implants are required to repair them.
At present, the new arthroscopic techniques and anchoring systems achieve a very solid and stable fracture union, improving recovery time , usually ranging from 2 to 4 months.
It is necessary to carry out an initial phase of rest that ranges between 2 and 4 weeks. Subsequently, physiotherapy is carried out to improve the shoulder joint’s mobility and musculature.
Irreparable Rotator Cuff Tear Treatment
When the rupture is massive, with stage 3 or 4 fatty degeneration and muscle atrophy, a latissimus dorsi flap in a motivated young patient is recommended, provided that the subscapularis tendon is present.
In a patient over 70, a biceps tenotomy is proposed after ineffective functional treatment. A biceps tenotomy is the cutting of the long biceps to reduce anterior pain under arthroscopy.
For other more complex forms, a modification of the shoulder functions by placing an inverted prosthesis is indicated. This prosthesis will use the upward forces of the deltoid muscle to transform them into rotational forces.
In case of a rotator cuff tear, the best is to consult experts with a distinguished history in complex surgical and nonsurgical procedures. The Orthopedic Surgeons team at the Burjeel Hospital for Advanced Surgery, Dubai, certified and Fellowship-trained, are the leading experts in performing complex shoulder surgeries with immense experience in treating all upper limb conditions due to arthritis or sports injuries. Call +971 800 55 or visit our website to book an appointment today!